Oral test product Portfolio
Real Time PCR test based on DNA extraction and Multiparametric quantification of DNA biomarkers and Mass Mectrometry VOC identification
The proposed biomarkers for oral and dental applications
- Bacteria
- Candida Albicans
- Total Oral Bacteria Count
- Viruses: HPV, Herpes, EBV…
- Saliva VOC identification in saliva
- Dental Clinic environment monitoring: Legionella Pneumophila, Pseudomonas aeruginosa in dental unit water, E.coli , Candida, MRSA
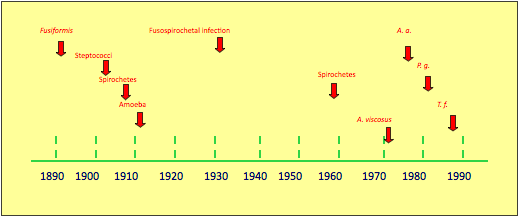
Historical timeline – Oral bacteria strains
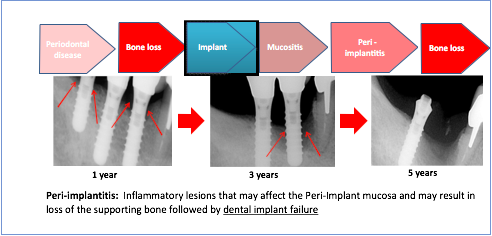
Prevalence of peri-implantitis
- 28-56% of patients have peri-implantitis at one or more implants.
- (Zitzmann & Berglunch, 2008)
Prevalence of bone loss
- 16% of patients / 6.6% of the implants HAVE ≥1.8mm bone loss after 1 year of implantation. (Roos-Jansaker et al., 2006a)
- 28% of patients have progressive bone loss over 5 years of post-implantation. (Fransson et al., 2005)
Institut clinident test: Perio-analyse® Real time pcr for peri-implantitis prevention
- DNA Extraction from paper points
- DNA amplification with DNA probes and primers
- Quantification per microbial target (% for each target /Total Oral Count)
- Total Oral Count
Perio-Analyse ® is a Real Time PCR test based on microbial DNA extraction and Multiparametric quantification of DNA bacterial specific sequences from Gingival Crevicular Fluid or Perio-implant Sulcus Fluid.
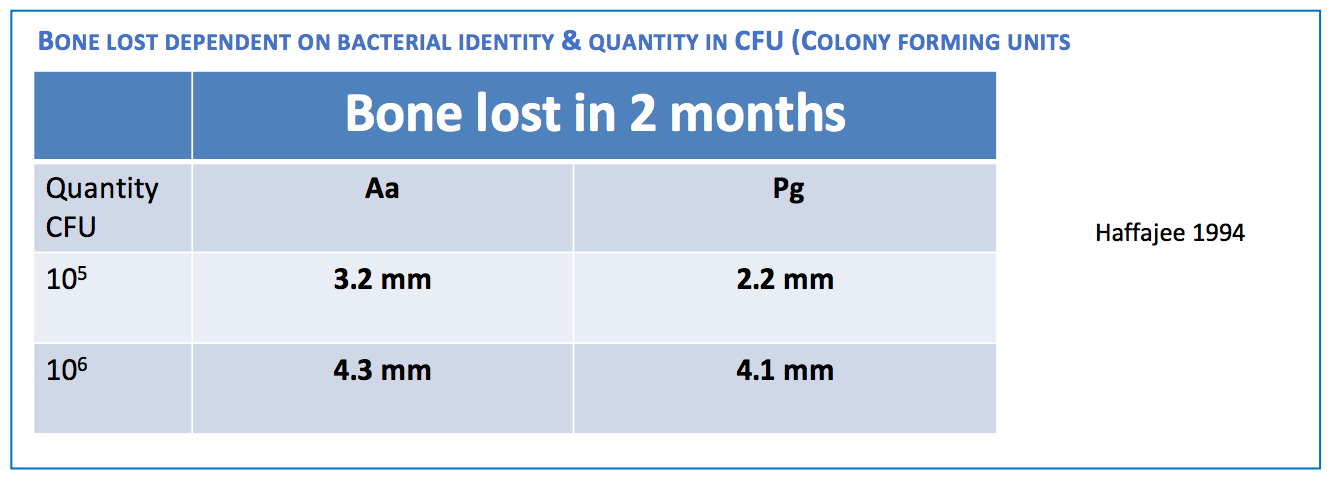
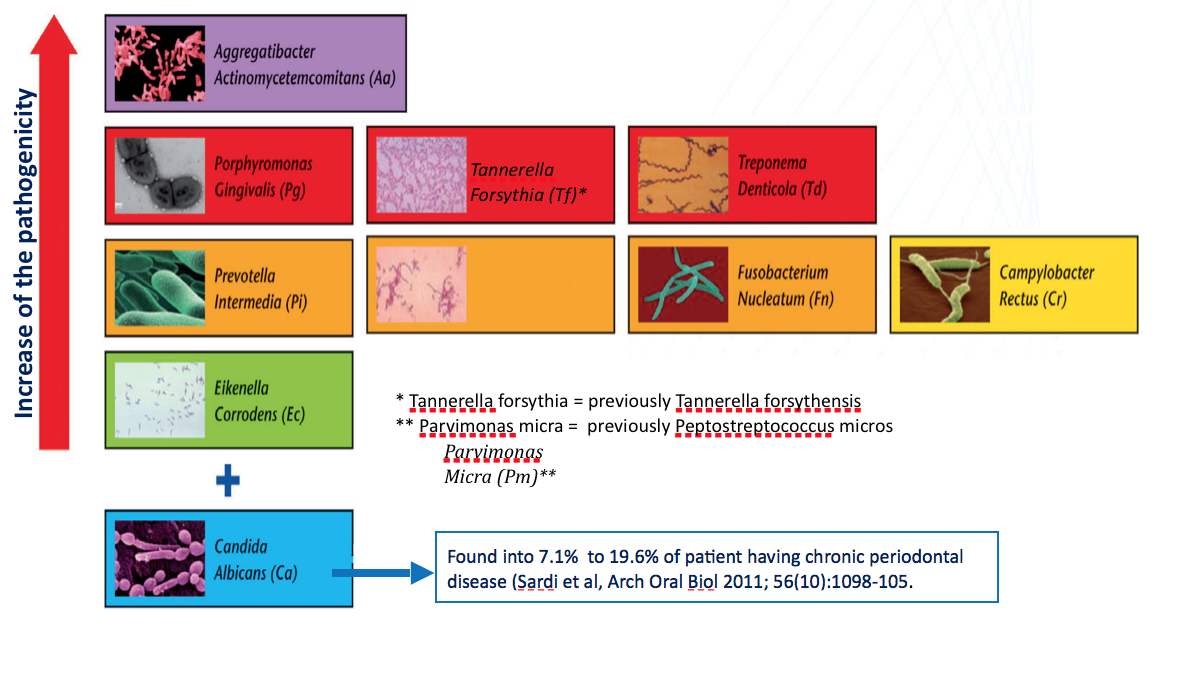
The proposed test is measuring 9 bacteria + Candida Albicans + Total Oral Count:
- Aggregatibacter actinomycet-emcomitans
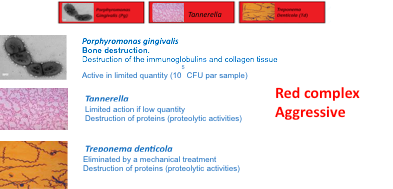
- Porphyrom-onas gingi-valis
- Tannerella forsythensis
- Treponema denticola
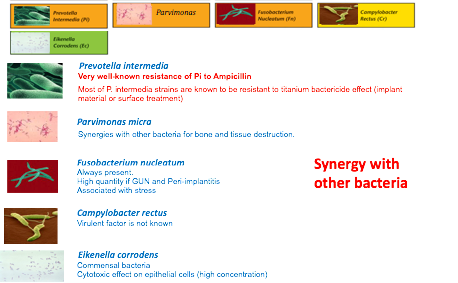
- Prevotella intermedia
- Peptostreptococcus micros
- Fusobacterium nucleatum
- Campylobacter rectus
- Eikenella corrodens
- Candida Albicans
- + Total Oral Bacteria Count
Same bacteria & microflora
(Mombelli 2002, Quirynen 2002,Renvert 2006,Mattout 2009,Pye
- Mucositis ≈ Gingivitis
- Peri-implantitis ≈ Periodontal disease
- Aa could be alone with high quantity in agressive periodontal disease
- Aa can not be treated only mechanically (intra-cellular bacteria)
- Bone and tissue destruction even in low quantity
- Specific antibiotic treatment, (Tetracycline) associated with mechanical treatment (new quinolone is also efficient). Metronidazole is not efficient.
- Osteoplasty could be recommended for total elimination (intra-cellular)
- Synthesis of endotoxins able to damage leucocytes & monocytes
- Present in endocardites and pneumonia

- C. albicans is commensal and a constituent of the normal flora comprising microorganisms that live in the human mouth
- Candida albicans can colonize sulcus and be responsible for periodontal disease
- Candida albicans cannot be treated with antibiotics (not a bacteria)
- C. albicans can colonize the periodontal pockets in patients with chronic periodontitis and patients with aggressive periodontitis.
- Antibiotic treatment could facilite development of Candida albicans
- Local antifungals could be recommended for elimination
- Precise quantification of Candida albicans is not possible
